In achalasia is a very rare disease which can make the person concerned to do with some complaints thoroughly. The doctor speaks of achalasia when there is a disorder in hollow organs with an occlusive function.
What is achalasia?
Schmatic presentation of the anatomy in achalasia. Click to enlarge.
The term achalasia is used to describe a disruption in the passage of food in the esophagus. The disease manifests itself primarily through swallowing disorders, which usually worsen as the disease progresses. For this reason, achalasia is divided into three stages: stage I (hypermotile form), stage II (hypomotile form) and stage III (amotile form).
In terms of frequency, the disease occurs very rarely. Only 1 in 100,000 people develop achalsia. It is not determined by age and gender. Anyone between the ages of 20 and 40 can theoretically participate in thisillness To suffer.
Causes
The causes of the disease cannot yet be named. Medicine divides the disease into primary and secondary achalasia. However, it is suspected that it is an autoimmune disease . In some patients with primary achalasia, for example, certain antibodies could be detected that have a negative effect on the autonomic nervous system .
It is also assumed that pathogens such as measles viruses , varicella-zoster viruses or human papillomaviruses may be the cause of an illness. Hereditary and psychological factors could also play a role. In general, the degeneration of nerve cells of the Auerbach myenterious plexus is responsible for the dysfunction of the esophagus. Inflammatory reactions often support degeneration.
Secondary achalasia can result from either carcinoma or Chagas disease, which is common in the tropics. A gastroenteritis and various other diseases around the digestive tract can be the cause of a secondary achalasia.
Symptoms, ailments & signs
A dysfunction of the esophagus can cause a variety of symptoms. Swallowing disorders and pain in the esophagus are typical. Sometimes the pain radiates into the chest and leads to increasing discomfort. Achalasia also leads to belching of undigested food, combined with heartburn and nausea .
At the beginning, the disease causes slight swallowing difficulties , which occur especially with solid food: The person affected has the feeling that the food is stuck in the throat. As the disease progresses, it is difficult for those affected to ingest liquid food. This can lead to deficiency symptoms, such as dizziness and tiredness .
In addition, food residues can get into the airways and cause other complaints such as pneumonia . Often, a dysfunction of the esophagus manifests itself through involuntary, mostly cramp-like pain behind the breastbone, which resembles heart problems . In the long run, achalasia leads to weight loss .
Outwardly, the disease manifests itself primarily in the characteristic signs of the disease, i.e. pale skin, sunken eye sockets and increased perspiration. The voice of the affected person is usually hoarse and fragile, which can give the impression of a cold . In severe cases, there may be a temporary loss of voice.
Diagnosis & course
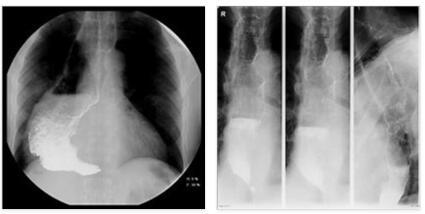
The diagnosis of achalasia is usually carried out in the early stages with a pressure measurement (manometry), which is carried out in several sections of the esophagus. The inadequate opening (relaxation) of the lower esophageal sphincter can be determined.
In addition, there is usually a disruption of the pumping function of the esophagus. In the late stages of the disease, the patient is given a barium porridge (contrast swallowable porridge). The findings can then be made by means of an X-ray examination . Routine diagnostics also include endoscopy of the upper digestive tract or a gastroscopy so that other causes of the disease can be excluded.
The course of the disease usually goes through all three stages. The hypermotile form of achalasia is characterized by the fact that the esophagus is still functional. However, it tries to pump against the high pressure in the lower sphincter muscle – the entrance to the stomach – and works overactive in the process. If the disease changes to the hypomotile form, the muscles of the esophagus are about to become sluggish, which is due to the expansion of the esophagus. In the amotile form, the end stage of the disease, the esophagus is, so to speak, defective and hangs like a flaccid muscle in the upper chest.
Often in the affected patients, due to the considerable swallowing disorders in the further course of the disease, a sometimes massive weight loss is noticeable. The general course of achalasia is usually very different and can be very rapid or even creeping. Treatment is important in both cases, otherwise the situation will worsen.
Complications
Achalasia can cause a variety of complications. If there is no treatment or if it is done too late, the esophagus will initially dilate. In extreme cases, this can lead to a so-called megaesophagus. The chyme can no longer be transported to the stomach, causing inflammation and other complications.
Typical for a megaesophagus is increased belching, irritable cough, hoarseness, and later pneumonia. Achalasia itself also increases the risk of esophageal cancer and its individual consequences. Comprehensive treatment can greatly reduce the risk of such complications, but the difficulty swallowing often persists for years.
This puts considerable strain on the entire throat, which can lead to infections and pain when eating, but also to an overload of the immune system. In less severe cases, an overloaded immune system can lead to tiredness and fatigue; in severe cases, chronic diseases and permanent damage to the internal organs develop from it. In the treatment of achalasia, allergic reactions, inflammations and other typical complications are possible, but usually the symptoms are alleviated without complications.
When should you go to the doctor?
If achalasia is suspected, medical advice is required in any case. A doctor’s visit is particularly urgent if the typical symptoms and signs persist over a longer period of time and increase in intensity and duration over the course of time. So, with constant weight loss or constant regurgitation, a doctor should be consulted quickly. If symptoms such as a dry cough, hoarseness and sore throat are added, there may already be a so-called megaesophagus, which must be treated immediately.
Pain when eating and infections in the mouth and throat indicate that the achalasia is already at an advanced stage. In this case, a medical clarification should take place as soon as possible in order to avoid a chronic development of the disease. In general, achalasia must always be medically clarified and treated. A doctor must therefore be consulted at the first suspicion of a serious illness. Patients at risk should have any conspicuous symptoms clarified by a specialist immediately.
Treatment & Therapy
Treatment of achalasia is always carried out with the aim of expanding the gastric entrance porter. Conservative, interventional and surgical therapies are possible for this.
In a conservative treatment with medication, means are used that reduce the muscle tension in the esophagus. Since the use of medication only has a minor influence on the symptoms of the disease, the conservative therapy method is usually only chosen in stage I of the disease and only if the affected patients cannot be treated interventionally or surgically.
Interventional therapy methods include balloon dilatation and botulinum toxin injection (BTX). Both treatment methods are carried out by means of a gastroscopy and therefore do not require an operation. With balloon dilatation, a balloon is inserted up to the narrowed stomach entrance and there, so to speak, “blown up”. However, with this method of treatment there is also the risk that many or even all layers of the esophagus will be destroyed. This procedure can also cause life-threatening inflammation. The treatment usually has to be carried out again after about one to five years.
Injection of botulinum toxin has now become a standard treatment. In this case, an agent is injected into the stomach entrance porter, which relaxes the muscle. In the short and medium term, the therapeutic successes are definitely positive, but not yet in the long term.
Muscle splitting, the Heller myotomy, has proven its worth as a surgical treatment method. As a rule, the so-called “open” surgical procedure, i.e. the abdominal incision, is used. With an abdominal incision, the long-term results are usually better than with the gentler laparoscopic technique. An operation on the muscles of the stomach entrance porter is usually the most successful treatment method in the long term.
Outlook & forecast
Achalasia is a chronic disease in which spontaneous healing can be ruled out. If the disease is left untreated, the typical swallowing difficulties usually increase. In the later course of the disease, the esophagus then gradually dilates , which can ultimately lead to a megaesophagus and severe lung and esophageal diseases.
However, if a diagnosis and treatment is carried out in the early stages of achalasia, the prognosis is positive. With the help of modern drugs and therapeutic measures, the symptoms can usually be sufficiently alleviated. An operation can counteract the sagging of the esophagus and alleviate the symptoms acutely. In the best case, the achalasia does not progress further after successful treatment or can at least be well controlled with the help of therapeutic measures and various drugs.
Since genetic factors are responsible for the development of achalasia, a prenatal examination is sometimes an option. This means that achalasia can be treated shortly after birth . Sick infants and young children have the prospect of esophageal surgery and, in most cases, will experience full recovery.
Prevention
Since the exact cause of achalasia has not yet been found, no effective prevention is known. By avoiding nicotine and alcohol , side effects such as esophagitis can be avoided. In general, doctors also advise that after successful treatment of achalasia, regular follow-up care should be carried out by endoscopy. This is the only way to identify possible late effects such as esophageal cancer in the early stages.
Aftercare
As a rule, aftercare is not possible in the case of achalasia. The disease must be treated by a doctor, because it does not heal itself and usually worsen the symptoms. The patient is mostly dependent on taking medication.
These should be taken regularly, although interactions with other drugs should also be taken into account. The person concerned should also avoid taking nicotine and alcohol if possible. In general, a healthy lifestyle with a healthy diet has a positive effect on the further course of the disease.
It is not uncommon for achalasia to be treated with surgical interventions. The affected person should rest after the procedure and take care of the body. In doing so, strenuous activities or sporting activities should be avoided. Furthermore, the patient’s stomach should also be spared.
Do not eat fatty foods. Since achalasia can also lead to cancer of the esophagus in some cases, the person affected should have regular examinations. Furthermore, contact with other sufferers of achalasia can also be useful, where stimulating information can be discussed.
You can do that yourself
Patients affected by achalasia suffer from a multitude of health complaints, most of which manifest themselves in food intake and digestion. Typical difficulties in eating, such as swallowing difficulties and frequent belching, can be alleviated with medicinal products.
The patient takes this before a meal, for example, whereby regular intake of the medication must always be agreed with the responsible specialist. It is often helpful if the patient directs his full attention to eating and swallowing while eating. This makes it easier to deal with swallowing difficulties and may reduce the risk of complications such as heavy swallowing.
The feeling of fullness typical of achalasia, especially after eating, is partially reduced by the selection of suitable foods. In this context, however, it is possible for the patient to achieve a healthier eating style at the same time . In addition, the person concerned reduces foods that often lead to a feeling of fullness after eating, such as very fatty foods.
On the other hand, with achalasia there is a risk of inadvertently losing body weight due to impaired food intake. In this case, the patient adheres to a meal plan drawn up by a doctor or a professional nutritionist to ensure adequate energy intake.