The bilirubin encephalopathy is a serious complication of hyperbilirubinemia in newborns. It is damage to the central nervous system. Serious consequential damage or even a fatal outcome are possible.
What is bilirubin encephalopathy?
Bilirubin encephalopathy is characterized by severe damage to the central nervous system (CNS), which is caused by increased bilirubin levels in newborns. The hyperbilirubinemia can a so-called kernicterus (jaundice with Hirnintoxikation) of the infant trigger. Free unconjugated bilirubin is insoluble in water. It only dissolves in fats. However, it is normally bound by certain albumins in the blood and transported to the liver.
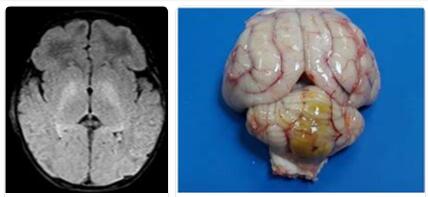
For various reasons, however, the binding capacity of the albumins can be overwhelmed, so that bilirubin accumulation in the blood occurs. Newborn jaundice develops, which in rare cases can be dangerous. If bilirubin crosses the blood-brain barrier, it can penetrate the core areas of the brain and develop neurotoxic effects there. The term kernicterus follows from this.
The basal ganglia, which are composed of putamen, globus pallidus and nucleus caudatus, are particularly affected by the damage. Severe bilirubin encephalopathy is often fatal. This complication occurs in 0.4 to 2.7 cases in every 100,000 live births in the western world. Due to less medical care, kernic terus is 100 times more common in some developing countries.
Causes
Bilirubin encephalopathy is caused by damage to certain core areas in the newborn’s brain through intoxication with unconjugated bilirubin. Unconjugated bilirubin is very often found free in the blood of newborns. Around 60 percent of all infants show symptoms of newborn jaundice, which usually heals within four days. Because the liver is still immature, bilirubin can often not be broken down as quickly. However, these symptoms are usually not of concern.
In rare cases, however, the bilirubin concentration becomes so high that free unconjugated bilirubin can cross the blood-brain barrier. There it has a neurotoxic effect and damages important core areas of the brain. Normally, the unconjugated fat-soluble bilirubin is bound to albumins, transported to the liver and broken down there. If there is an increased formation of bilirubin due to hemolysis in the case of blood group incompatibilities towards the mother, the binding capacity of albumin is overwhelmed. The bilirubin concentration in the blood increases very sharply and can cross the blood-brain barrier.
Various drugs also reduce the binding capacity of bilirubin to albumin through displacement processes. These include, for example, diazepam, sulfonamides, furosemide and others. Even if the bilirubin concentration in the blood is normal, the blood-brain barrier for bilirubin can become permeable. This often occurs with a lack of oxygen (hypoxia), low blood sugar (hypoglycaemia), excess blood acidity (acidosis) or hypothermia (hypothermia). Even if the albumin concentration is too low (hypoalbuminemia), bilirubin can be exceeded by the blood-brain barrier.
Symptoms, ailments & signs
Acute bilirubin encephalopathy usually has three phases:
- First of all, the infant’s unwillingness to drink, flaccid muscle tension, drowsiness and a sedentary lifestyle are determined.
- In a second phase, the newborn begins to scream shrilly. The consciousness becomes increasingly cloudy (stupor). In addition, there is increased muscle tension, resulting in hyperextension of the neck or spine.
- Eventually, muscle tension may increase, with cramps occurring. The stupor can go into a coma. The disease often ends fatally. However, if the infant survives the acute phase, there are often long-term effects with deafness, extrapyramidal motor movement disorders and psychosomatic developmental disorders.
The extrapyramidal motor movement disorders are known as athetosis and are expressed in involuntarily slow screwing movements of the feet and hands. The joints are overstretched. The corridor is stumbling and overshooting. The cause of these bizarre movements lies in the disruption of the interaction between antagonists and agonists.
Diagnosis & course
Elevated bilirubin levels are very common in the first few days of life. For this reason, screenings are carried out in the maternity clinics in order to avert the risk of bilirubin encephalopathy as early as possible by identifying a possible hyperbilirubinemia. When the baby turns yellow, the first signs of increased bilirubin levels appear. The bilirubin values are determined through the skin using a multispectral device in the first 20 hours.
If the values are critical, a blood test for hyperbilirubinemia should be done. It has been shown that neurological disorders can already occur at a value above 20 mg / dl. If treatment is not timed at this level, motor dysfunction can occur by the age of seven. With bilirubin concentrations above 25 mg / dl there is already a great risk of kernicterus.
Complications
An increased bilirubin level in the child initially leads to a yellowish coloration of the child (neonatal icterus), which is usually not bad and subsides again without any complications. In the worst cases, however, bilirubin can accumulate in the brain in the basal ganglia and thus lead to kernicterus, resulting in bilirubin encephalopathy. The infant is initially characterized by general weakness and muscular weakness.
This results in a reluctance to drink, whereupon the baby can dry out (desiccosis). This makes the skin more cracked and makes the baby more susceptible to infection. In addition, in the worst case, the heart can fail. In addition, the reflexes in the newborn are weakened.
In addition, the baby may suddenly start screaming in pain. In addition, there is a clouding of consciousness and cramping of the muscles, especially of the neck and spine (opisthotonus), so that the baby overstretched its head. In addition, the sunset phenomenon can reveal itself in the infant, which means that the eye turns downwards when opening and thus the range of vision is restricted.
In the worst cases, cerebral deficits occur in the child, which can have various consequences, such as deafness. In addition, there are usually more seizures and a mental development disorder. The disease can also lead to a coma and even death of the child.
When should you go to the doctor?
In most cases, bilirubin encephalopathy is diagnosed before birth or immediately after birth. For this reason, no additional diagnosis or treatment by another doctor is necessary. Treatment in the hospital must, however, take place immediately, as bilirubin encephalopathy can otherwise lead to death in the worst case.
In most cases, an exam should be done when the child has no muscle tension, is very sleepy and does not move. The child’s consciousness is also clouded and can thus indicate the disease. In severe cases, the children fall into a coma. In order to avoid complications or death later, a doctor should be alerted immediately in the event of these complaints.
In most cases, the diagnosis and treatment of bilirubin encephalopathy takes place directly in the hospital. As a rule, parents do not need to see an additional doctor for this. A positive course of the disease cannot be guaranteed in every case.
Treatment & Therapy
If bilirubin values are very high above 20 mg / dl, treatment must be initiated immediately to avoid bilirubin encephalopathy. The treatment takes place within the first 72 hours through phototherapy with blue light. The wavelength of blue light is between 425 and 475 nanometers.
During phototherapy, the unconjugated water-insoluble bilirubin is converted into water-soluble lumirubin. This is then excreted from the body via the bile or the kidneys. If the bilirubin values are above 30 mg / dl, phototherapy will no longer help. Then a blood transfusion should be done.
Outlook & forecast
The prognosis of bilirubin encephalopathy depends on how quickly therapy is started after the onset of symptoms of the disease or when bilirubin levels are increased.
Even before the onset of the disease, the infant must be constantly monitored in order to be able to react quickly if the concentration of unconjugated bilirubin exceeds 15 mg / dl. When unconjugated bilirubin crosses the blood-brain barrier into the brain, it destroys the nerve cells there by blocking phosphorylation reactions.
These processes are potentially irreversible. This means that they can no longer be reversed or only partially reversed. During the treatment, the water-insoluble, unconjugated bilirubin is converted into water-soluble conjugated bilirubin by means of blue light and can thus be excreted from the body via blood exchange transfusions.
If no treatment is given, long-term effects can occur, the symptoms of which can only be alleviated with symptomatic therapies. These long-term effects include motor disorders, numbness, constant seizures and mental retardation. The motor disorders are expressed, among other things, by screw-like movements of the extremities. The later damage is the more serious the later treatment begins. However, treatment that starts immediately after the onset of the disease does not guarantee that there will be no long-term damage.
Since increased bilirubin levels are very common in newborns, early screening after birth is very important in order to detect and treat hyperbilirubinemia (increased bilirubin concentration in the blood) in good time.
Prevention
Bilirubin encephalopathy can only be prevented by screening early after birth. If the bilirubin values are very high, blue light treatment must be carried out immediately, or if the values are extremely high, a blood exchange transfusion must be carried out. If jaundice occurs after a few days at home and the child falls into lethargy, a doctor should be consulted immediately.
Aftercare
As a rule, those affected with bilirubin encephalopathy do not have any special means of follow-up care available. In the worst case scenario, this disease can also lead to a fatal outcome, with the child dying. Early diagnosis and therapy have a very positive effect on the further course of the disease and can avoid various complications.
As a rule, the patient depends on exposure to blue light to alleviate the symptoms. If there is no treatment, the child often dies immediately. Further follow-up care for bilirubin encephalopathy relates in most cases to the newborn child and not to the mother. The child needs special support to deal with mental retardation and further retarded development.
The seizures can also be relieved with the help of various medications. Parents must ensure that they are taken regularly, and interactions with other medications should also be taken into account. After the birth, the child is dependent on regular examinations. Since bilirubin encephalopathy can also lead to psychological complaints in the parents and relatives of the child, intensive discussions and contact with other sufferers of bilirubin encephalopathy are also very helpful here.
You can do that yourself
The possibilities for self-help are very limited with bilirubin encephalopathy. The disease occurs in newborns. Naturally, they cannot take any measures to improve their situation. Therefore, the consequences of the disease usually have to be borne by relatives and parents. These are exposed to helplessness due to the circumstances and have to regulate their own emotional states.
If this cannot be achieved on one’s own, psychological assistance should be sought. Immediate medical care for the newborn is important. A close exchange with the treating doctors and nurses is necessary so that we can react as quickly as possible to changes in the state of health.
In addition, relatives should be adequately informed about the disease and inform themselves. The consequences and disturbances are individual, but to a highly life-impairing extent. Keep calm so that good and optimal decisions can be made that are in the interests of the offspring.
Unity and mutual strengthening among family members is advisable so that no conflict of interest emerges and offices or authorities have to be involved. Disputes, self-interest or power games ultimately damage the well-being of the newborn and lead to time delays when doctors need the consent of the parents for the treatment methods.