According to abbreviationfinder, HLHS stands for Hypoplastic Left Heart Syndrome. The term hypoplastic left heart syndrome summarizes a severely underdeveloped left heart and several other serious heart defects associated with it in newborns, which mostly affect the mitral and aortic valves. Survival after birth in these children initially depends on maintaining the prenatal short circuit between the pulmonary and systemic circulation via the ductus arteriosus and the foramen ovale. This allows the right ventricle to take over the function of the left ventricle to a certain extent.
What is Hypoplastic Left Heart Syndrome?
Important initial and simple diagnostic tools when a hypoplastic left heart syndrome is suspected are, in addition to measuring pulse, blood pressure, temperature and respiratory rate, listening to the heart sounds with a stethoscope and measuring oxygen saturation.
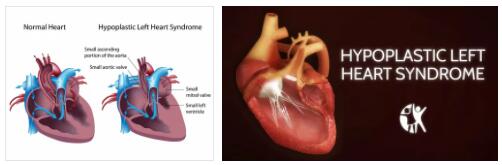
The main feature of hypoplastic left heart syndrome (HLHS) is a severely underdeveloped system of the left ventricle in newborns. The left ventricle sometimes only reaches the size of a pea and therefore inevitably remains functionless.
The occurrence of HLHS is associated with other serious heart valve defects and usually also a hypoplastic malformation of the initial part of the large artery (aorta) up to and including the aortic arch. The aorta normally arises from the left ventricle of the heart. The survival of a newborn with HLHS is initially dependent on maintaining the circuit between the systemic and pulmonary circulation.
It is present before birth and is only gradually closed after birth with the release of the pulmonary circulation with the first breath. The malformation of the left ventricle (left heart ventricle) usually also causes a malformation with loss of function of the mitral and aortic valves.
In a healthy heart, the mitral valve establishes the connection between the left atrium and left ventricle, and the aortic valve prevents blood from flowing back from the aorta into the left ventricle during the relaxation phase of the ventricles, diastole.
Causes
The causes of hyperplastic left heart syndrome have not (yet) been clearly clarified. Many indications, above all a familial accumulation, speak for a causation by genetic defects. Other factors such as drug use or alcohol abuse, which are also suspected, have not yet been proven.
Bacterial or viral infectious diseases that women suffer during pregnancy are also clearly excluded as the cause of HLHS. Depending on the author, hypoplastic left heart syndrome accounts for around two to nine percent of all congenital heart defects.
Symptoms, Ailments & Signs
Children born with hypoplastic left heart syndrome typically show few symptoms at first. This is due to the fact that their circulation in the first few days of life does not differ significantly from that of healthy babies.
The still open ductus arteriosus, which creates a connection between the pulmonary and body circulation, mixes the oxygen-rich and the oxygen-poor blood of the two circulations. Only in rare cases does a premature blue discoloration (cyanosis) occur in newborns with HLHS due to lack of oxygen.
Healthy babies only experience relief when the ductus arteriosus closes, while HLHS babies experience acute oxygen deficiency because the blood that is pumped from the right ventricle into the pulmonary circulation can no longer reach the systemic circulation.
Within the first two days of life, the affected babies develop respiratory distress syndrome with rapid and labored breathing and shortness of breath. Fatigue sets in very quickly and the performance of the newborn is greatly reduced.
Diagnosis & course of disease
Important initial and simple diagnostic tools when a hypoplastic left heart syndrome is suspected are, in addition to measuring pulse, blood pressure, temperature and respiratory rate, listening to the heart sounds with a stethoscope and measuring oxygen saturation. The electrocardiogram (ECG) and especially the ultrasound examination provide information about the heart function.
A chest X-ray provides clarity about the location and size of the heart. In exceptional cases, a magnetic resonance imaging (MRT) or a heart catheter examination is necessary. If left untreated, the course of the disease in all known forms leads to death within a few days if the ductus arteriosus closes “properly” so that there is no longer a connection between the lungs and the systemic circulation.
The right ventricle can then no longer supply the systemic circulation with blood. After a successful operation in several, time-staggered steps, life expectancy is good. Except for competitive sports, an almost normal life can be led.
Complications
The left heart syndrome leads to a very serious complication which, if left untreated, leads to the death of the child. Artificial maintenance of bodily functions is usually necessary for the patient to survive with this disease. As a rule, there are no particular complaints or symptoms in the first few days.
However, the skin can also turn blue due to the lack of oxygen. This undersupply also has a negative effect on the patient’s internal organs and can embellish them. This leads to shortness of breath and further to shortness of breath. The patient’s resilience decreases enormously. The lack of oxygen can also lead to loss of consciousness or a coma. If left untreated, the patient eventually dies.
Early diagnosis and treatment can prevent complications. This usually requires an operation, which, however, is successful and resolves the symptoms. The life expectancy is brought back to normal as a result of the intervention. Usually, the patient can lead an ordinary life, although certain sports may not be able to be practiced.
When should you go to the doctor?
If a newborn’s skin turns blue, seek immediate medical attention. The blue color indicates a lack of oxygen in the organism. Without medical care, the infant is at risk of premature death. If there is an acute lack of oxygen, the emergency doctor must be called. In the event of shortness of breath, respiratory arrest or gasping, immediate intervention is required. First aid measures must be taken so that the newborn child survives this acute condition. If you notice any breathing abnormalities within the first two days after birth, you should consult a doctor.
During a stay in the hospital, the nursing staff should be informed of the observations as soon as possible. If the respiratory rate increases, if the child needs significantly more force to breathe, or if breathing seems difficult overall, a doctor must be called. If the baby shows a reduced performance level in direct comparison to infants of the same age, a doctor should be consulted.
A doctor’s visit is also necessary if the newborn has an unusually strong need for sleep or shows renewed signs of fatigue very quickly after a longer period of sleep. If the child becomes apathetic, the muscle tension decreases or if conspicuous movement restrictions are evident, a doctor should be consulted. Clarification of the complaints is necessary to prevent a collapse.
Treatment & Therapy
The only effective treatment method is a multi-stage operation. The first and most important goal is to maintain the connection between the pulmonary and systemic circulation that is present at birth, so that the right ventricle can supply the body with mixed blood.
In the Norwood surgical method, the pulmonary artery (arteria pulmonalis) is connected to the surgically reconstructed ascending part of the aorta, and the pulmonary circulation is supplied by the so-called Blalock-Taussig shunt. In a later second operation (Norwood 2), the right pulmonary artery is connected to the superior vena cava.
This ensures that the pulmonary circulation is supplied with blood almost passively by the pressure in the venous part of the circulation and can be enriched with oxygen. In this second intervention, the previously inserted Blalock-Taussig shunt is removed again.
In a third operation, the inferior vena cava is also connected to the pulmonary arteries. This ensures that all of the venous blood from the systemic circulation flows into the pulmonary circulation and the right heart takes over the supply of the systemic circulation.
Prevention
There are no known preventive measures that could prevent hypoplastic malformation of the left ventricle. Since there is no reliable evidence as to whether drug use or alcohol abuse can cause hypoplastic development of the left ventricle, abstinence from drugs, alcohol and cigarettes is generally recommended, but cannot prevent the occurrence of HLHS.
If the disease has already been diagnosed in family members, a diagnosis can be made in a prenatal ultrasound examination. In the positive case, the birth should then be transferred to a specialized children’s clinic, which can carry out the necessary interventions after the birth.
Aftercare
The treatment of hypoplastic left heart syndrome is followed by individual follow-up, which mostly deals with artificial respiration and nutrition. The infants react positively to the presence and loving care of their parents. After the therapy, the children often succeed in leading a relatively normal life after an initially difficult phase.
However, regular medical examinations are necessary throughout life in order to identify problems in good time. Depending on the individual case, the doctor’s recommendations can lead to patients abstaining from strenuous sports. This avoids overstressing the cardiovascular system.
In connection with the disease, there are no prophylactic measures that have been medically proven. However, it makes sense to avoid drugs and alcohol, even if there is no known direct connection. If the disease has run in the family before, parents should have a prenatal screening done.
If the diagnosis is positive, they can react quickly and register for the delivery date in a specialized clinic. Everything is already prepared here for the necessary interventions shortly after the birth. A certain caution and a health-conscious lifestyle quickly become a habit for the family and the patients themselves.
You can do that yourself
Hypoplastic Left Heart Syndrome affects newborn infants who are unable to take care of themselves. Therefore, in the case of the disease, the parents or guardians play the essential role in promoting the prospect of recovery and the quality of life of the patient. It is crucial for a positive outcome of the disease that the parents observe the newborn child closely and contact a doctor immediately if there are any abnormalities during the first few days of life. If the parents fail to seek emergency medical care or if this occurs too late, the baby usually dies.
The newborn suffers from hypoplastic left heart syndrome with a blue discoloration of the skin, which indicates a lack of oxygen. Furthermore, the physical well-being of the child patients is enormously impaired by shortness of breath. If such observations are made, the parents immediately call an ambulance and keep the child alive with first aid measures.
In the hospital, the patient is given artificial respiration and feeding, and the presence of the parents usually has a positive effect on the infant’s condition. If the therapy is successful, the child is usually able to lead a normal life, with lifelong check-ups by the doctor. Some patients refrain from special sports due to medical instructions in order not to overload the circulatory system.